Port Authority of Leixões Contingency Plan
1. INTRODUCTION
-
Located in the Porto Metropolitan Area, the Port of Leixões serves a hinterland of 14 million inhabitants. Recognized as a port of the Core Network of the Trans-European Transport Networks (TEN-T), it is the second largest port in Portugal in terms of tonnage handled and the largest port in the northwest of the Iberian Peninsula.
As a gateway port, it plays a strategic role in the national economy by providing multimodal transport solutions and essential services for the businesses in the northern region of the country. It facilitates the flow of finished products and the supply of raw materials and consumer goods, thus playing a crucial role in the competitiveness and internationalization of Portuguese companies.
Situated in an urban area that generates a trade surplus of €5 billion in its goods transaction balance, it encompasses the 16 Portuguese municipalities with the highest export strength. Containerized cargo bound for 182 countries worldwide is shipped from here, with an annual throughput of approximately 20 million tons.
As a multipurpose port, it offers diverse operational infrastructures, including terminals for solid and liquid bulk, container terminals, multipurpose terminals, a petroleum terminal, a roll-on/roll-off terminal, a commercial marina, a fishing port, and two cruise terminals, serving approximately 100,000 passengers annually.
These factors, combined with the ease of international movement of people and cargo and the speed at which it occurs, result in significant human mobility. This includes not only the daily participants in port operations and services but also a large number of crew members and passengers of various nationalities, intersecting in the port area and its surroundings. The presence of passenger ships, carrying a high number of people in confined spaces, adds to the complexity of the sanitary risk at the Port of Leixões.
In terms of health risk, the Port of Leixões thus presents a complex situation, underscoring the need for a border epidemiological surveillance system that enables early and effective intervention, as well as adequate alert and response capabilities, in an articulated and integrated manner. This applies to both pandemic threats and situations of physical risk that pose or may pose an increased risk to human health.
-
The World Health Organization, a specialized agency of the United Nations responsible for international health matters and public health, approved the fourth revision of the International Health Regulations (IHR) in May 2005. This revision identifies a set of procedures necessary for assessing public health in a cross-border context and reflects the international community's concern about the potential health, social, economic, and environmental consequences of epidemic spread.
The IHR, with the latest revision in force since June 15, 2007, is a legal instrument binding 194 countries. Its aim is to assist the international community in preventing and responding to public health risks that have the potential to cross borders and threaten populations worldwide.
As a State Party to the International Health Regulations, Portugal is bound by its provisions. Annex I-(B) of the regulations defines the minimum requirements that Designated Airports and Ports must meet. It mandates, in subparagraph (a) of paragraph 2, the obligation to ensure an appropriate response to public health emergencies by establishing and maintaining a contingency plan for public health emergencies, including the designation of a coordinator and contact points at entry points, public health services, and other relevant entities and services.
Therefore, the Port of Leixões, in fulfilling its responsibilities as a Designated Port, has developed the present Contingency Plan of the Port Authority of Leixões (PCAPPL). This plan outlines the measures, particularly operational ones, to be implemented in the event of undesired events that may endanger the lives or health of the Port Community, in coordination with:
- With the Port Health Authority and all local agencies involved in responding to public health emergencies, particularly those integrated into the CCOPPL (Port of Leixões Protection Operations Coordination Center).
- The Occupational Health Services of APDL, responsible for the defense and protection of its active employees, both in the port and administrative staff.
- With various port stakeholders, notably its Concessionaires, whose plans are integrated and coordinated with this Plan.
The Port Health Plan of Porto de Leixões is an integral part of the "PCPL - Port of Leixões Contingency Plan, by the Matosinhos Municipal Health Authority - International Health," which is responsible for testing and managing this plan in an integrated manner. This responsibility is centered on Dr. Jaime Batista, the Coordinator of the Matosinhos Public Health Unit, and his team, who are available 24 hours a day at the port health unit in Porto de Leixões.
The coordination of port intervention is thus ensured by the Health Authority, Dr. Jaime Batista, in coordination with the Port Protection Officer (OPPL) - Commander Rui Cunha.
.
- With the Port Health Authority and all local agencies involved in responding to public health emergencies, particularly those integrated into the CCOPPL (Port of Leixões Protection Operations Coordination Center).
-
After three meetings within the span of a week, the World Health Organization (WHO) declared on January 30, 2020, that the coronavirus outbreak should be classified as a Public Health Emergency of International Concern (PHEIC). On February 11, the disease caused by the 2019-nCoV was given the new designation of COVID-19 (Coronavirus Disease - 2019).
This Contingency Plan was developed within the framework of this PHEIC, following the recommendations of the World Health Organization (WHO) and the Norms and Guidelines of the Directorate-General of Health (DGS), namely Guideline No. 005/2020 of 26/02/2929 - Procedures for Ports and Travellers via Maritime Routes, and Guideline No. 006/2020 of 26/02/202 - Prevention, Control, and Surveillance Procedures in Companies, in coordination with the Matosinhos Public Health Unit - Maritime Health, and the APDL Occupational Health Services.
2. AIMS OF THE PLAN (PCAPPL)
-
The present Port Contingency Plan (PCAPPL) aims to minimize the effects of events posing an increased risk to public health within the scope of port operations. It ensures the coordination and harmonization of procedures among the various authorities of the Port of Leixões to effectively respond to any situation deemed by the Health Authority (HA) as a public health emergency, particularly in combating the spread of COVID-19, whether on board a ship present or entering the Port of Leixões or within its port facilities.
It serves as an Operational Plan outlining a set of procedures and operational guidelines to be implemented under the coordination of the Port Operations Department (OPPL), responsible for coordinating port intervention. This occurs in constant coordination and under the guidance of the Health Authority, responsible for coordinating health intervention within the port area.
-
- To prepare in advance an appropriate and coordinated response with other authorities of the Port of Leixões and all stakeholders in port operations, namely the Concessionaires
- To respond appropriately and cohesively to a public health emergency.
- To enhance the capacity for detecting and swiftly responding to public health emergency situations related to COVID-19
- Clear definition of the information chain, command, and controlo
- Standardize routines and define procedures.
- Minimize the impact of the event considered a public health emergency.
- Enhance the forecasting, alert, and response system.
- Ensure the continuity of port activity.
- To prepare in advance an appropriate and coordinated response with other authorities of the Port of Leixões and all stakeholders in port operations, namely the Concessionaires
3. FORECAST AND ALERT SYSTEM / RISK SCENARIOS
-
The procedures associated with the various alert levels aim to anticipate or early detect events in order to prevent, control, and minimize their negative impacts, even enabling decision-making regarding actions to be implemented before the ship docks, in response to a reported case identified on board.
They are fundamental elements for the risk analysis prior to the arrival of the ship, reception of notifications sent from the ship, communication with other ports preceding the ship's call, other authorities at the local, regional, and national levels, and assessment of the risk level that the previously called ports may pose before the ship's arrival.
Ships originating from affected areas may pose a health risk, so information about affected areas as well as temporary or definitive recommendations issued by the WHO can contribute to identifying events and deciding on the type of sanitary measures to apply.
All routine procedures, such as Free Practice, Health Clearance, requests for inspections, health visits, are conducted through the Electronic Platform (JUP/JUL).
-
- The ship's captain notifies the Port Health Authority through the port information system (JUP) of health risks, a communication conveyed by the Maritime Health Declaration (MHD) (IHR Article 37), explicitly addressing sanitary issues on board, identified in the 8 mandatory fields on the MHD form.
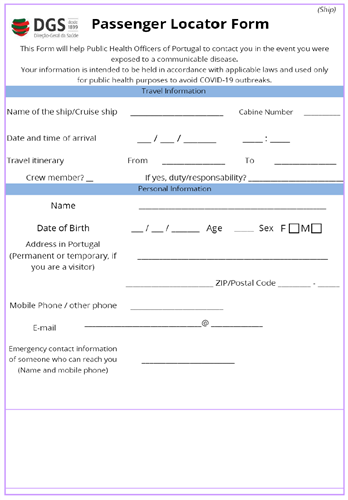
- In order to ensure that all operational services involved in the planning and authorization of the ship's entry are informed of the possibility of any of the 8 mentioned fields being positive, thus potentially constituting a situation of elevated sanitary risk, a functionality of Automatic Notification was implemented to the entire Port Health Authority team, the Port Authority services, notably the OPPL, and other authorities (SEF/GNR/PORT CAPTAINCY). (Image 1)
Declaração Marítima Saúde: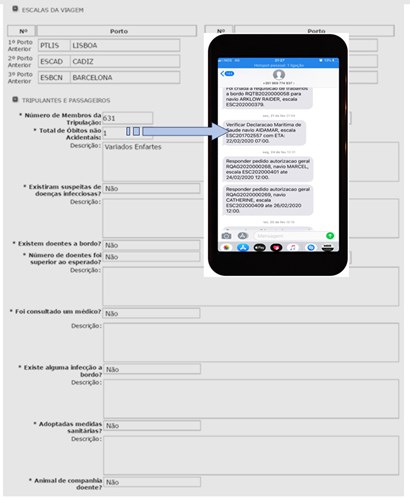
Image 1 - Automatic Notification to the Port Health Authority and Port Authorities- Whenever any of the fields has a positive response (other than 0)
- The entry maneuver will be carried out after analysis by the Port Health Authority, with the OPPL informed of the decision, while maintaining the signaling of this entity as Red (Semaphore).

- The ship's captain notifies the Port Health Authority through the port information system (JUP) of health risks, a communication conveyed by the Maritime Health Declaration (MHD) (IHR Article 37), explicitly addressing sanitary issues on board, identified in the 8 mandatory fields on the MHD form.
-
Ships originating from affected areas may pose an increased risk for the spread of COVID-19. Therefore, the prior analysis of the ports called before their arrival at Leixões and the travel times are fundamental data for a case-by-case analysis and for the eventual need to promote additional protective actions, both in the port facility and for services directly interacting with crews and passengers (Pilots / Boat Crews / Terminal Operators, etc.)
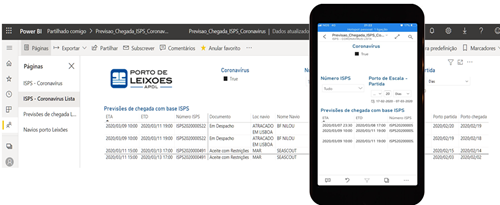
Image 2 - Application for analyzing previously called ports and travel times
In order to conduct prior assessment before the arrival of ships and take any additional protective actions, or to support decision-making in coordination with the Port Health Authority and other authorities and stakeholders in port operations and services, an application (APP) was developed for analyzing all ships announced for the port. This app creates alerts for ships coming from ports of risk, providing information on the length of stay in those ports and the time of travel until arrival at Leixões. (Image 2). -
With potentially several days between the introduction of the Maritime Health Declaration (MHD) into the port information system (JUP) and the ship's arrival at the port, the vessel traffic service (VTS) identifies the ship at least two hours before arrival. They ensure that there are no changes to the onboard health status and that it aligns with the prior notification in the MHD.
In the event of any changes, the Port Planning Service and the Port Protection Officer of Leixões are immediately informed. The Port Protection Officer then notifies the Port Health Authority, and the authorization semaphore is set to red.
4. RISK SCENARIOS / ALERT LEVELS
-
Risk scenarios and their consequent alert levels depend on situations that may contribute to increased health risk for crew and/or passengers of ships arriving or docked at the Port of Leixões, as well as for any stakeholders in port operations who are in direct contact with the ship or the port community.
The need to activate organizational structures for an adequate and timely response is based on risk assessment by the Health Authority. Activation levels for structures and stakeholders are established, along with the mobilization of human and material resources, according to the level of threat:
The activation phases of the Plan are established according to the risk level.
Phase 1 - Pre-pandemic period - Attention (situational) - Green Alert Level
In this phase, there were reports of possible isolated cases due to imported transmission in Portugal. It corresponds to the occurrence of national or international public health events that may be of interest to partners. These events are usually monitored and managed locally. The port area remains in normal activity, with no alerts about occurrences or events that may pose an increased risk to crew/passengers, port agents, and/or the population.Phase 2 - Concern phase - Yellow Alert Level
This corresponds to the moment of exponential resurgence of infected individuals worldwide, a situation that threatens the normal functioning of organizations. Public health events emerge that require a coordinated response involving additional resources at the regional and/or national level. The port area records the occurrence of one or more cases among crew and/or passengers with little significant impact. The situation is controllable with the adoption of active measures.Phase 3 - Operational phase
This corresponds to the moment of exponential appearance of infected individuals in the area, anticipating that, in addition to the actions outlined in previous phases, it may be necessary to mobilize extra resources at the regional and national levels. The threat is real, corresponding to a Public Health Emergency of National Importance. The port area experiences occurrences of several cases among crew and passengers and/or within the port community and population. There is a need to suspend mobility in the port area and/or prohibit entry of ships, with the need to define essential minimum services.Risk communication
Communication to partners and the population is the responsibility of the Health Authority and will be ensured in coordination with other authorities.
5. OPERATIONAL RESPONSE AND COORDINATION STRUCTURE
-
With regards to human and organizational resources, the implementation of actions included in the PCAPPL requires a concerted effort from all APDL services and efficient coordination and communication with the Port Health Authority, Different Port Entities, and the Port Community in order to meet the necessary standards of efficiency:
- All operational services of APDL and ship service providers are active and on standby 24/7, 365 days a year, at the contacts available in the contact lists:
- VTS - Vessel Traffic Service - Navigation Control
- Piloting and Tug Service
- Navigation and service planning and coordination
- Security control center and video surveillance
- The Port Protection Officer (OPPL) is permanently reachable, directly or through the services mentioned above, which are directly under their responsibility.
- Maritime Health in Leixões operates 24/7, 7 days a week, ensured by a core team with specific training and in permanent attendance, consisting of:
- Coordinator - Dr. Jaime Baptista
- Doctor - Dr. Nuno Rodrigues;
- TSA - Fátima Sousa and Miguel Maia;
- Nurses - Sérgio Sousa and Teresa Cardoso.
All routine procedures, including Free Practice, Health Clearance, requests for inspections, and health visits, are carried out through the Electronic Platform (JUP/JUL).In an emergency situation, although the JUP/JUL remains the primary registration platform, direct contact via telephone with the Authorities and other involved entities will be prioritized.
This plan is coordinated with the Contingency Plan of the Port of Leixões of the Municipal Health Authority of Matosinhos (PCPL), therefore communication between the involved entities follows the procedures outlined therein, utilizing highly streamlined communication channels.
-
Suspected Case Definition (Guidance 006/2020)
The following definition is based on the information available, as of the date, from the European Centre for Disease Prevention and Control (ECDC), and should be adopted by companies.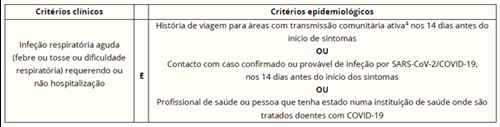
Image 3Areas with active community transmission as of 25.02.2020:
Asia: China, South Korea, Japan, SingaporeMiddle East: Iran
Europe: Regions of Italy - Emiglia-Romagna, Lombardy, Piedmont, and Venetoo
I. SUSPECTED CASE - SHIP DOCKED AT THE PORT OF LEIXÕES
- If a person on board the ship identifies a suspected case (crew member or passenger), they immediately inform the Captain.
- The Captain immediately contacts the Shipping Agent or VTS on channel 12.
- The Shipping Agent contacts the Health Authority (Maritime Health Service) of the port and informs APDL-OPPL (Port of Leixões Port Protection Officer), or the Planning Service, or VTS.
- OPPL or VTS informs the Captaincy and the SEF.
Boarding or disembarking is immediately prohibited, except for Health Authorities / INEM, with normal access resuming only with explicit authorization from the Port Health Authority.
THE HEALTH AUTHORITY ASSESSES THE SITUATION AND, IF CONFIRMING SUSPICION:
- Provides initial guidance for the patient to be placed in isolation. The patient should be separated from other crew members and passengers and restrict activities outside their cabin. A sanitary facility should be designated for the patient's exclusive use.
- Directs to provide the patient with a surgical mask. The mask should be worn by the patient and properly fitted.
- Immediately calls the Doctor Support Line of the Directorate-General of Health (DGS) (300 015 015) for validation of suspicion.

FiguRE 4II. IF THE CASE IS NOT VALIDATED by the Doctor Support Line of the DGS
The situation is closed for COVID-19, and usual procedures for managing an onboard patient appropriate to the clinical situation should be activated.III. IF THE CASE IS VALIDATED by the Doctor Support Line of the DGSS
The following indications for managing a suspected COVID-19 case on board should be followed:- Only one designated crew member should provide assistance to the patient.
The patient should be kept isolated on board, wearing a surgical mask if their clinical condition allows, until the arrival of the National Institute of Medical Emergency (INEM) team activated by the DGS. - If the ship is docked, the INEM team may board the ship and ensure the patient's disembarkation to transport them from the port to the reference hospital.
- Entry of any person into the cabin or isolation area where the patient was located is prohibited until cleaning and disinfection procedures are completed, or until the laboratory result is negative. This prohibition can only be lifted by the Health Authority.
- Information on close contacts of the patient should be collected using the Passenger Location Card (PLC) (Annex I of OT no. 005/2020).
Close contacts on board are defined as:
Individuals who have had direct contact with the patient (e.g., family members, travel companions (cabinmates), or individuals who provided assistance, or others defined by the Health Authority). -
- If the ship contacts VTS or is contacted by VTS to report a sick person on board, VTS instructs the ship to contact MRCC (Maritime Rescue Coordination Center), while simultaneously establishing contact with this service.
- VTS immediately alerts Maritime Health and the Captaincy, informing CCN (Ship Control Center), which will then contact OPPL, providing them with the information.
- No pilot will be appointed to carry out the maneuver without explicit authorization from Maritime Health and without the knowledge of OPPL.
- The Maritime Search and Rescue Coordination Center (MRCC) coordinates with CODU-Mar (Maritime Medical Coordination Center).
- The doctor on duty at CODU-Mar contacts the Doctor Support Line to validate the case.
- All procedures previously described in the port are applied (activation of the INEM team for patient transport, in coordination with the Port Health Authority).".
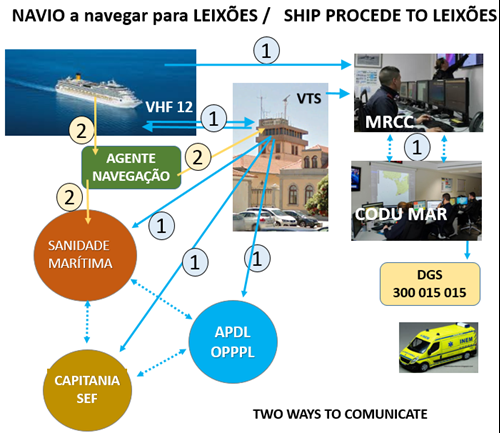
Figura 5 -
The Maritime Search and Rescue Coordination Center (MRCC) coordinates with CODU-Mar.
The doctor on duty at CODU-Mar contacts the Doctor Support Line to validate the case. If the case is validated, MRCC coordinates with the designated Maritime Health Authority (on national duty rotation) to support decision-making regarding the port of arrival (Leixões), ensuring the most effective management of the patient and their transmission to the Captain.
Once the destination port (Leixões) is determined, the Maritime Health Authority informs the doctor at the DGS Doctor Support Line, who activates the Regional Health Authority with jurisdiction in the geographic area of the destination port.
The Regional Health Authority should inquire with the Health Authority of the destination port to obtain information regarding the terminal and docking area of the ship. This specific information regarding the ship's name and docking berth should be communicated to the Maritime Authority, which in turn provides the necessary information to the INEM team, ensuring the patient's disembarkation and transportation from the port to the reference hospital.
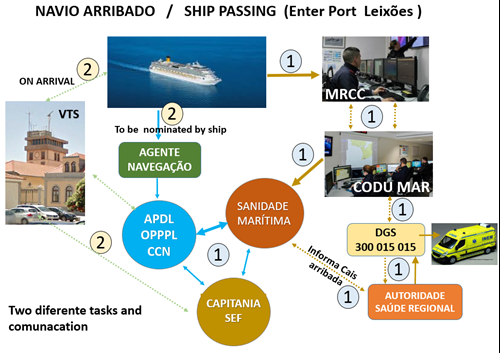
Figure 6- If the ship intends to make port, it should appoint a Shipping Agent who will request entry authorization from the various authorities through the port information system (JUP). The Harbor Master must issue the arrival declaration.
- The entry maneuver can only be scheduled after authorization from Maritime Health in coordination with OPPL, ensuring the most suitable dock for the potential patient disembarkation or facilitating the entry of health services on board.
- The Maritime Declaration of Health (Annex 8 of the International Health Regulations) must be entered into the electronic platform.
- Free Pratique for a ship with a suspected case of COVID-19 can only be issued after the situation is evaluated by the Health Authority.
- If the ship intends to make port, it should appoint a Shipping Agent who will request entry authorization from the various authorities through the port information system (JUP). The Harbor Master must issue the arrival declaration.
6. SUSPECTED CASE AT THE PORT FACILITIES
-
Each port facility has its own plan in which dedicated isolation rooms are identified. Therefore, in the event of any suspicion, the Facility's Plan will be activated by its Facility Protection Officer (OPIP) or another responsible party for the Plan, immediately informing the OPP and following the communication flow depicted in Figure 7.
Any member of the port community who identifies a person fitting the definition of a suspected COVID-19 case at the port facilities should contact their supervisor.
.
- The management informs the Facility Protection Officer (OPIP).
- The OPIP contacts the Port Protection Officer (OPP).
- The OPP contacts the Health Authority.
The Health Authority assesses the situation, and if it confirms the suspicion
- The Health Authority provides the following initial instructions:
- Provide the patient with a surgical mask, if their clinical condition allows. The mask should be worn by the patient themselves and properly adjusted.
- Direct the patient to the isolation room/area defined in the port's contingency plan, with access to a dedicated sanitary facility.
In the port's isolation area, the Health Authority (see Annex):
- Performs symptomatic assessment and epidemiological investigation.
- Immediately calls the Doctor Support Line of the Directorate-General of Health (DGS) to validate the suspicion.
- Activates the procedures outlined in the port's Contingency Plan for managing suspected COVID-19 cases:
- Restrict access to the area/space of the port where the patient stayed (until they are directed to the isolation room) for subsequent cleaning and disinfection.
- Lifts the restriction only upon approval from the Health Authority.

Figura 7 - The management informs the Facility Protection Officer (OPIP).
-
- The situation is closed for COVID-19, and the usual procedures for managing patients at the port facilities, appropriate to the clinical situation, should be activated.
-
- The patient should be kept in the isolation room/area (with a surgical mask) until the arrival of the INEM team, activated by the DGS.
- The Health Authority initiates epidemiological investigation and identifies close contacts of the patient:
- Passengers sharing the same cabin on the ship;
- Travel companions of the patient.
- Other close contacts who were on board the ship (see definition above).
- Individuals who provided assistance to the patient at the port facilities.
- The patient should be kept in the isolation room/area (with a surgical mask) until the arrival of the INEM team, activated by the DGS.
-
- The Directorate-General of Health (DGS) informs the Regional Health Authority of the laboratory results.
- The Regional Health Authority informs the Health Authority of the port.
- The Health Authority of the port informs the Port Protection Officer and the Harbor Master, and:

Figure 8If the case is negative for COVID-19:
The Health Authority of the port determines:- The deactivation of the procedures from the suspected COVID-19 case management phase of the Port Contingency Plan, previously activated.
- Lifts the access ban to the cabin/isolation area.
If the case is positive for COVID-19:
The cabin/isolation area must remain isolated until the cleaning and disinfection procedures are validated by the Health Authority.
The Health Authority of the port must communicate the sanitary measures taken on board the ship and/or at the port facilities to the Regional Health Authority.. - The Directorate-General of Health (DGS) informs the Regional Health Authority of the laboratory results.
-
Upon confirmation of a case, in addition to the previously described procedures, the procedures for active contact tracing as outlined in section 5.2 of DGS Guideline No. 002/2020, dated 25/01/2020, updated on 10/02, should also be activated.
-
After a journey with a confirmed case on board a ship, the following aspects should be considered:
- After the departure of the patient, cleaning and decontamination procedures must be ensured.
- Cleaning should be carried out by professionals trained in the use of Personal Protective Equipment (PPE) (gown, mask (preferably FFP2), cap, goggles with lateral protection, and single-use gloves, in accordance with Guidance No. 03/2020 dated 30/01/2020.
- Compressed air equipment should not be used due to the risk of aerosol recirculation.2
- Cleaning and disinfection should be reinforced, especially on frequently touched surfaces, particularly those close to the patient and more likely to be contaminated. Special attention should be given to the cabin where the case was located (e.g., table/trays and other materials/equipment used by the patient).
- Single-use cleaning equipment should be used. If equipment is for multiple uses, it should be cleaned and disinfected after each use.
- The application of disinfectants should be preceded by cleaning.
- Cleaning and disinfection of surfaces should be performed with:
- Degreasing detergent, followed by
- The appropriate disinfectant according to the manufacturer's recommendations.
- The treatment of bed linens/towels and dishes used by the patient should follow the procedures outlined in Guidance No. 03/2020 dated 30/01/2020.
- Biological waste (including hand wipes, tissues) should be placed in a plastic bag that, after sealing, should be stored in a rigid container and sent for incineration, or another similar method in terms of effectiveness.
- The above recommendations also apply to the isolation area and other potentially contaminated areas of port facilities.
- After the departure of the patient, cleaning and decontamination procedures must be ensured.
-

1 - South Cruise Terminal - APDL
2 - Multipurpose Terminal - TCL-Leixões Container Terminal
3 - Border Health Delegation - APDL
4 - South Container Terminal - TCL-Leixões Container Terminal
5 - General Cargo Terminal - TCGL-Leixões General Cargo Terminal
6 - North Passenger Terminal - APDL
7 - North Container Terminal - TCL-Leixões Container Terminal
8 - Pilots Building (Occupational Health) - APDL
9 - Tanker Terminal - Galp -
HEALTH AUTHORITY
- Jaime Baptista
Coordinator Health Delegate
jaime.baptista@ulsm.min-saude.pt
912790552 - Health Authority - Scale
ups@ulsm.min-saude.pt
917920292
APDL
- Rui Cunha
OPPL - Port Protection Officer
rui.cunha@apdl.pt
965863605 - Luís Barros
OPIP - Port Facility Security Officer
luis.barros@apdl.pt
965237983 - Lino Antunes
OPIP - Port Facility Protection Officer
lino.antunes@apdl.pt
927244543 - Manuel Teixeira
Head of Occupational Health Division
manuel.teixeira@apdl.pt
961622629 - André Ferreira
Occupational Health Division
andre.ferreira@apdl.pt
934903721 - VTS - Vessel Traffic Service
vts@apdl.pt
229990700 - CCN - Ship Coordination Center
ccn@apdl.pt
229990700
HARBOUR MASTER´S OFFICE
- Rui Silva Lampreia
Deputy Harbour Master, Port of Leixões
capleixoes.of.adj@amn.pt
916353115
MARITIME POLICE
- Elísio Silva
2º local Commander
cardoso.silva@marinha.pt
916353222 - Duty Team
policiamartima.leixoes@amn.pt
clpm.leixoes@amn.pt
916353249
SEF
- João Gomes
Border Crossing Supervison
joao.gomes@sef.pt
961750131
- Jaime Baptista
-